A device designed to reduce noise generated by internal combustion engines utilizing water as a cooling and/or exhaust gas conditioning medium is the focal point of this discussion. These components are often employed in marine applications and specialized industrial settings. Their purpose is to abate the sharp, percussive sounds associated with engine operation, contributing to a quieter operational environment. A typical example involves routing the engine’s hot exhaust gases through a chamber containing water, leading to cooling and a reduction in volume.
The utilization of these specialized exhaust systems offers several advantages. A primary benefit is noise reduction, improving working conditions for personnel and minimizing disturbance to surrounding areas. Additionally, the cooling effect reduces the temperature of the exhaust gases, mitigating the risk of fire hazards and potentially allowing for safer disposal of the exhaust. Historically, the need for these systems arose from the increasing demand for quieter and more environmentally conscious engine operation, particularly in confined spaces and environmentally sensitive locations.
The subsequent sections will delve into the specific designs, operational principles, applications, and maintenance considerations associated with these systems. Further examination will address the various types available, their performance characteristics, and the factors that influence their selection for a particular application.
Operating Considerations for Water-Cooled Exhaust Dampening Systems
The following guidance outlines critical factors for the effective and reliable operation of these systems.
Tip 1: Material Compatibility: Ensure that the materials used in the construction of the exhaust system are compatible with both the exhaust gases and the cooling water. Corrosion due to dissimilar metals or unsuitable materials can lead to premature failure.
Tip 2: Water Quality Monitoring: Regularly assess the quality of the cooling water. Impurities, such as sediment or excessive mineral content, can reduce cooling efficiency and accelerate corrosion. Implement filtration or water treatment procedures as necessary.
Tip 3: Proper Sizing and Installation: Verify that the size of the dampening system is appropriate for the engine’s exhaust volume and flow rate. Incorrect sizing can lead to back pressure, reducing engine performance, or inadequate noise suppression. Adherence to manufacturer specifications during installation is essential.
Tip 4: Temperature Regulation: Maintain exhaust gas temperatures within acceptable limits. Overheating can damage the system and compromise its noise reduction capabilities. Implementing temperature monitoring and control measures is advisable.
Tip 5: Regular Inspection and Maintenance: Conduct periodic inspections of the system, checking for leaks, corrosion, and blockages. Regular cleaning and maintenance can prolong the system’s lifespan and ensure optimal performance.
Tip 6: Prevention of Backflow: Implement measures to prevent backflow of water into the engine in the event of system failure or improper shutdown. Backflow can cause significant engine damage.
Tip 7: Monitoring of Exhaust Pressure: Track the exhaust pressure within the system. Elevated pressure may indicate a blockage or other malfunction that requires immediate attention.
Adherence to these operational considerations ensures the longevity, efficiency, and safety of water-cooled exhaust dampening systems, contributing to a quieter and more reliable engine operation.
The concluding section will summarize the key advantages and future trends in the development of these technologies.
1. Noise Reduction Effectiveness
Noise reduction effectiveness is a primary performance metric for water exhaust mufflers. The ability to substantially decrease engine exhaust noise is crucial in various applications, including marine vessels, power generation facilities, and industrial settings, where noise pollution is a significant concern.
- Acoustic Absorption Mechanisms
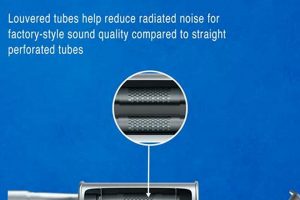
Acoustic absorption mechanisms within a water exhaust muffler attenuate sound waves through a combination of processes. These include diffusion, reflection, and absorption. Water, as a medium, facilitates sound wave dissipation due to its density and thermal properties. The design of the muffler influences the efficiency of these mechanisms; baffled chambers and strategically placed water jets are frequently employed to maximize sound wave interaction and energy conversion into heat.
- Frequency-Specific Attenuation
Engine exhaust noise comprises a spectrum of frequencies. Effective noise reduction necessitates addressing this entire spectrum, not just the dominant frequencies. Water exhaust mufflers are often designed to target specific frequency ranges, tailoring their effectiveness to the unique noise characteristics of the engine. Advanced designs incorporate features that alter the resonant frequencies, minimizing noise amplification in the audible range.
- Backpressure Considerations
While noise reduction is paramount, it must be balanced against engine backpressure. Excessive backpressure impedes exhaust flow, reducing engine performance and fuel efficiency. The design of a water exhaust muffler directly influences backpressure; overly restrictive designs compromise performance. Optimization involves achieving effective noise attenuation without significantly increasing backpressure. Computational fluid dynamics (CFD) is frequently used to model and refine muffler designs to minimize backpressure.
- Material Selection and Longevity
The effectiveness of noise reduction is directly linked to the materials used in the muffler’s construction. Corrosion-resistant materials are essential, especially in marine environments. Over time, corrosion can degrade the muffler’s structural integrity, leading to leaks and reduced noise attenuation. Furthermore, the material’s acoustic properties influence its ability to absorb or dampen sound waves. Stainless steel and specialized polymers are commonly used due to their durability and acoustic performance.
In summary, the noise reduction effectiveness of a water exhaust muffler is a complex interplay of acoustic principles, design considerations, and material properties. Effective mufflers offer substantial noise attenuation while minimizing backpressure and ensuring long-term durability. Continuous advancements in materials science and acoustic engineering are driving the development of more efficient and environmentally sound water exhaust muffler technologies.
2. Corrosion Resistance
Corrosion resistance is a paramount design consideration in water exhaust mufflers. The operational environment inherently exposes these systems to corrosive agents, necessitating robust material selection and protective measures to ensure longevity and consistent performance. The continuous interaction of exhaust gases, water, and potentially aggressive chemical compounds creates a highly corrosive atmosphere that can rapidly degrade susceptible materials.
- Material Selection: Alloys and Composites
The selection of appropriate materials forms the cornerstone of corrosion resistance. Austenitic stainless steels (e.g., 316L) are frequently employed due to their inherent resistance to chloride-induced pitting and crevice corrosion, common in marine applications. Alternative materials, such as high-nickel alloys or fiber-reinforced polymers, offer enhanced corrosion resistance in exceptionally aggressive environments. The selection process involves a careful evaluation of the specific operating conditions and the anticipated exposure to corrosive agents.
- Protective Coatings: Enhancing Surface Integrity
Protective coatings provide an additional layer of defense against corrosion. These coatings, which may include epoxy resins, ceramics, or specialized metallic coatings, create a barrier between the base material and the corrosive environment. The effectiveness of the coating depends on its adherence, impermeability, and resistance to degradation under the operating conditions. Regular inspection and maintenance of these coatings are crucial to ensure their continued protection.
- Galvanic Corrosion: Mitigation Strategies
Galvanic corrosion occurs when dissimilar metals are in electrical contact in the presence of an electrolyte. This phenomenon can accelerate the corrosion of the more anodic metal. Mitigation strategies include the use of sacrificial anodes, electrical isolation, and the selection of compatible materials with similar electrochemical potentials. Careful design and installation practices are essential to prevent galvanic corrosion in water exhaust muffler systems.
- Water Quality: Impact and Control
The quality of the water used for cooling and exhaust gas conditioning significantly affects corrosion rates. Impurities, such as chlorides, sulfates, and dissolved gases, can accelerate corrosion. Implementing water treatment processes, such as filtration, deionization, or chemical inhibitors, helps to minimize corrosion. Regular monitoring of water quality is essential to ensure the effectiveness of the treatment program.
The integration of these corrosion-resistant strategies is essential for the reliable and long-lasting performance of water exhaust mufflers. Neglecting these considerations can lead to premature system failure, increased maintenance costs, and potential environmental consequences. Advances in materials science and corrosion engineering continue to drive the development of more durable and corrosion-resistant water exhaust muffler technologies.
3. Thermal Management
Thermal management is intrinsically linked to the design and operation of water exhaust mufflers. These devices rely on water’s heat absorption capacity to cool exhaust gases, mitigating thermal stress on downstream components and reducing the risk of fire hazards. Effective thermal management directly influences the system’s performance, efficiency, and longevity.
- Exhaust Gas Temperature Reduction
The primary function of thermal management within a water exhaust muffler is to lower the temperature of exhaust gases. By directly contacting hot exhaust with water, a significant amount of thermal energy is transferred, reducing gas temperatures from several hundred degrees Celsius to levels closer to ambient. This temperature reduction protects sensitive materials in downstream components, such as flexible exhaust hoses or fiberglass structures, from heat damage and degradation. Examples include marine exhaust systems where excessively hot exhaust can ignite nearby combustible materials.
- Water Consumption and Heat Transfer Efficiency
The rate of water consumption is a key parameter in thermal management. Insufficient water flow results in inadequate cooling, potentially leading to overheating and component failure. Conversely, excessive water flow can reduce engine efficiency and increase operational costs. The design of the water exhaust muffler, including the internal baffling and water injection methods, directly impacts the heat transfer efficiency. Well-designed systems maximize heat transfer with minimal water consumption, optimizing both cooling performance and resource utilization.
- Prevention of Steam Formation and Backpressure
The rapid cooling of exhaust gases can lead to steam formation within the muffler. Excessive steam generation can increase backpressure on the engine, negatively affecting performance. Effective thermal management strategies must mitigate steam formation while ensuring adequate cooling. This can be achieved through optimized water injection techniques, gradual cooling processes, and efficient steam separation mechanisms within the muffler. Examples include pulse-tuned exhaust systems where precise control over gas flow is critical.
- Material Selection for Thermal Stability
The materials used in the construction of water exhaust mufflers must withstand significant temperature gradients and thermal cycling. Repeated heating and cooling can induce thermal stress, leading to material fatigue and eventual failure. Materials with high thermal conductivity and low coefficients of thermal expansion are preferred to minimize stress concentrations. Examples include the use of stainless steel alloys designed to maintain structural integrity at elevated temperatures and resist thermal cracking.
In conclusion, thermal management is a critical aspect of water exhaust muffler design and operation. Effective cooling minimizes component stress, reduces fire hazards, optimizes engine performance, and extends system lifespan. The integration of efficient heat transfer mechanisms, optimized water consumption strategies, and thermally stable materials is essential for reliable and safe operation.
4. Engine Backpressure and Water Exhaust Mufflers
Engine backpressure, the resistance to exhaust flow, is a critical parameter affecting engine performance and longevity. The integration of a water exhaust muffler introduces additional complexities regarding backpressure management due to the device’s inherent design and operational characteristics.
- Muffler Design and Flow Restriction
The internal design of a water exhaust muffler, intended to facilitate noise reduction and exhaust gas cooling, inevitably introduces flow restrictions. Baffles, water injection nozzles, and expansion chambers create resistance to the free flow of exhaust gases, contributing to backpressure. An improperly designed muffler can generate excessive backpressure, hindering engine efficiency and potentially causing damage over time. The design must therefore balance noise attenuation and cooling efficiency with the need to minimize flow restriction.
- Water Accumulation and Blockage
The presence of water within the exhaust system presents the risk of accumulation or blockage, further increasing backpressure. Incomplete drainage or improper system orientation can lead to water pooling within the muffler, impeding exhaust gas flow. Solid debris, such as scale or rust particles, can also accumulate and exacerbate blockages. Regular maintenance and inspection are essential to prevent water accumulation and ensure unobstructed exhaust flow.
- Engine Performance and Fuel Efficiency
Elevated backpressure directly impacts engine performance. Increased resistance to exhaust flow reduces the engine’s ability to expel combustion gases effectively, leading to decreased power output and fuel efficiency. In extreme cases, excessive backpressure can cause engine overheating, pre-ignition, and damage to exhaust valves and other engine components. Monitoring exhaust pressure is crucial for identifying and addressing potential backpressure issues promptly.
- System Optimization and Mitigation Strategies
Effective management of engine backpressure in water exhaust muffler systems requires a multi-faceted approach. Optimized muffler designs, incorporating streamlined flow paths and efficient water separation mechanisms, are essential. Regular maintenance, including cleaning and inspection, helps prevent water accumulation and blockages. The selection of appropriate muffler size and configuration, tailored to the specific engine characteristics, is also critical for minimizing backpressure. Furthermore, incorporating backpressure monitoring devices allows for real-time assessment and proactive intervention.
The careful consideration and management of engine backpressure are essential for ensuring the reliable and efficient operation of systems incorporating water exhaust mufflers. Design optimization, preventative maintenance, and continuous monitoring are crucial strategies for mitigating the adverse effects of backpressure and maximizing engine performance.
5. Water Consumption Rate
Water consumption rate is a pivotal parameter governing the performance and operational efficiency of water exhaust mufflers. It directly impacts cooling effectiveness, noise reduction capabilities, and overall system longevity. The balance between adequate water supply and efficient resource utilization is essential for optimal operation.
- Cooling Efficiency and Exhaust Gas Temperature
The water consumption rate directly dictates the cooling efficiency of the muffler. A higher rate facilitates more effective heat transfer, resulting in lower exhaust gas temperatures. Insufficient water supply leads to inadequate cooling, potentially causing thermal stress on downstream components and increasing the risk of fire hazards. Examples include marine applications where prolonged operation with insufficient water flow can damage exhaust hoses or fiberglass structures. The required water consumption rate is typically calculated based on the engine’s power output and exhaust gas temperature.
- Noise Attenuation and Water-Gas Interaction
Water consumption rate also influences the muffler’s noise attenuation capabilities. The interaction between water and exhaust gases is a primary mechanism for noise reduction. A higher rate increases the surface area of contact between the two media, enhancing sound wave dissipation and absorption. However, excessively high water flow can lead to increased backpressure and reduced engine efficiency. The optimal water consumption rate strikes a balance between noise attenuation and engine performance.
- Material Corrosion and Water Chemistry
The water consumption rate indirectly affects the corrosion rate within the muffler. A continuous flow of water helps to flush away corrosive byproducts and prevent the buildup of scale or deposits. However, the water’s chemical composition also plays a significant role. Impurities, such as chlorides or sulfates, can accelerate corrosion. Monitoring and controlling water quality, along with appropriate water consumption rates, are crucial for minimizing corrosion and extending the muffler’s lifespan. Examples include the use of sacrificial anodes in marine systems to mitigate galvanic corrosion.
- System Design and Water Management
The design of the water exhaust muffler influences the optimal water consumption rate. Efficient designs minimize water usage while maximizing cooling and noise attenuation. Features such as optimized baffling, water injection nozzles, and drainage systems contribute to efficient water management. Properly sized water pumps and flow control valves ensure consistent and adequate water supply. Furthermore, closed-loop cooling systems, which recirculate water, can significantly reduce overall water consumption compared to open-loop systems.
Therefore, careful consideration of the water consumption rate is essential for the efficient and reliable operation of water exhaust mufflers. Balancing cooling performance, noise attenuation, corrosion resistance, and system design ensures optimal results across diverse applications. Continuous advancements in muffler technology are focused on minimizing water consumption while maximizing performance and longevity.
6. Material Durability
Material durability is a foundational element in the design and performance of water exhaust mufflers. These systems are subjected to a confluence of stressors, including high temperatures, corrosive environments, and mechanical vibrations, each placing significant demands on the materials from which they are constructed. The ability of these materials to withstand such stressors over prolonged periods directly dictates the muffler’s service life and operational reliability. Failure to adequately address material durability leads to premature degradation, system failure, and potential safety hazards. For instance, the marine environment, with its high salinity, accelerates corrosion in susceptible materials, necessitating the use of specialized alloys or protective coatings to maintain structural integrity.
The selection of materials for water exhaust mufflers involves a careful evaluation of several factors, including corrosion resistance, thermal stability, and mechanical strength. Austenitic stainless steels, such as 316L, are frequently employed due to their inherent resistance to chloride-induced pitting and crevice corrosion. However, even these materials may require additional protection in particularly aggressive environments. Protective coatings, such as epoxy resins or ceramic layers, can provide an added barrier against corrosion. Furthermore, the design of the muffler itself plays a crucial role in mitigating stress concentrations and minimizing the risk of mechanical failure. Proper welding techniques and stress-relieving processes are essential for ensuring the long-term durability of the system.
In summary, material durability is an indispensable aspect of water exhaust muffler technology. The selection of appropriate materials, coupled with robust design and manufacturing practices, is paramount for ensuring reliable performance and extended service life. Overlooking material durability considerations results in increased maintenance costs, reduced operational efficiency, and potential safety risks. Continuous research and development efforts are focused on identifying and implementing advanced materials and protective technologies to further enhance the durability of water exhaust muffler systems in diverse and demanding operating environments.
7. System Integration
The operational efficacy of a water exhaust muffler is inextricably linked to its seamless integration within the broader engine and exhaust system. Proper system integration ensures the muffler functions optimally, delivering intended noise reduction, exhaust cooling, and emission control without compromising engine performance or overall system reliability. Mismatched components or improper installation can negate the benefits of even the most advanced muffler design, leading to reduced efficiency, increased maintenance requirements, and potential system failures. For example, a muffler designed for a specific exhaust flow rate, when installed on an engine producing a significantly different flow, will likely result in either inadequate noise reduction or excessive backpressure, negatively impacting engine performance.
System integration encompasses several crucial considerations. These include proper sizing of the muffler to match engine displacement and operating parameters, ensuring compatibility of materials between the muffler and other system components to prevent galvanic corrosion, and implementing appropriate drainage mechanisms to prevent water accumulation. Furthermore, correct placement and support of the muffler within the system are vital to minimize vibration and stress on connections. Marine applications, in particular, demand meticulous attention to system integration due to the corrosive environment and the potential for water intrusion. Failure to adequately integrate a water exhaust muffler into a marine propulsion system can lead to significant operational challenges and costly repairs.
In conclusion, system integration is not merely an ancillary consideration but a fundamental requirement for the successful deployment of water exhaust mufflers. A holistic approach, encompassing careful component selection, meticulous installation practices, and ongoing maintenance, is essential for realizing the full potential of these devices. Effective system integration maximizes performance, enhances reliability, and contributes to the overall longevity of the engine and exhaust system, ensuring compliance with noise regulations and promoting environmental responsibility.
Frequently Asked Questions
This section addresses common inquiries regarding water exhaust mufflers, providing concise and factual answers to enhance understanding of these specialized systems.
Question 1: What constitutes a water exhaust muffler, and how does it function?
A water exhaust muffler is a device designed to reduce noise generated by internal combustion engines by routing exhaust gases through water. The water absorbs sound energy and cools the exhaust, reducing both noise and temperature.
Question 2: In what applications are water exhaust mufflers typically employed?
These mufflers are commonly utilized in marine applications, power generation facilities, and industrial settings where noise reduction and exhaust cooling are critical requirements.
Question 3: What are the primary benefits associated with the use of water exhaust mufflers?
Key benefits include noise reduction, reduced exhaust gas temperature, mitigation of fire hazards, and compliance with noise regulations.
Question 4: What materials are commonly used in the construction of water exhaust mufflers?
Materials frequently employed include stainless steel (e.g., 316L), specialized alloys, and fiber-reinforced polymers, selected for their corrosion resistance and thermal stability.
Question 5: What maintenance procedures are essential for water exhaust mufflers?
Essential maintenance includes regular inspection for leaks and corrosion, cleaning to prevent blockages, and monitoring water quality to minimize corrosion.
Question 6: How does a water exhaust muffler affect engine performance?
A properly designed water exhaust muffler minimizes backpressure, thereby preserving engine performance and fuel efficiency. Excessive backpressure can reduce power output and increase fuel consumption.
The effective utilization of water exhaust mufflers hinges on selecting appropriate designs, implementing consistent maintenance, and meticulously monitoring operational parameters.
The subsequent sections will explore advanced design considerations and future trends in water exhaust muffler technology.
Conclusion
This exploration has detailed the essential characteristics of the water exhaust muffler. The analysis encompasses noise reduction effectiveness, material durability, thermal management considerations, and the complexities of system integration. Comprehension of these facets is crucial for appropriate selection, implementation, and sustained operation across diverse applications.
Continued research and development remain paramount. Enhanced material science, optimized designs, and rigorous maintenance protocols will ensure the long-term viability and efficacy of the water exhaust muffler as a critical component in noise mitigation and environmental responsibility. The ongoing pursuit of these advancements is vital for meeting increasingly stringent regulatory standards and fostering a more sustainable operational landscape.