A perceived reduction in sound clarity, often described as dull or indistinct audio, can significantly impact auditory experiences. This altered perception might present as if sounds are filtered or distant, making it difficult to discern details and nuances. An example is listening to music where individual instruments blend together, losing their distinct character.
Accurate auditory perception is critical for communication, environmental awareness, and enjoying various forms of entertainment. When sounds lack clarity, individuals may experience difficulties understanding speech, misinterpreting warnings, or finding music and other audio sources less enjoyable. Historically, issues with clear sound reception have driven advancements in acoustics, audio technology, and medical understanding of hearing health.
Several factors contribute to a decline in auditory fidelity. These can range from physical obstructions in the ear canal and auditory processing issues to environmental conditions and technological limitations of sound reproduction equipment. The following sections will explore these potential causes in greater detail.
Addressing Reduced Auditory Clarity
When audio appears indistinct, several troubleshooting steps can improve the listening experience. Identifying the source of the perceived lack of clarity is essential for implementing effective solutions.
Tip 1: Assess Ear Canal Obstructions: Examine the ear canal for wax build-up. Excessive cerumen can physically impede sound waves from reaching the eardrum. Consult a healthcare professional for safe wax removal if necessary.
Tip 2: Evaluate Equipment Connections: Verify that all audio cables are securely connected. Loose or damaged cables can cause signal degradation, leading to a loss of sound detail and clarity. Replace any suspect cables.
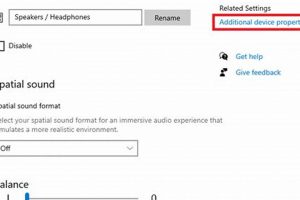
Tip 3: Check Audio Settings: Review the audio settings on playback devices and software. Ensure that equalization settings are not inadvertently suppressing certain frequencies or applying filters that diminish overall sound quality. Resetting to default settings can often resolve unintended alterations.
Tip 4: Analyze Playback Source Quality: Low-resolution audio files or compressed streaming services can result in reduced audio fidelity. Compare the sound to a known high-quality source, such as a lossless audio file, to determine if the issue originates from the source material.
Tip 5: Evaluate the Acoustic Environment: Room acoustics can significantly affect sound perception. Excessive reverberation or echoes can create a sensation of indistinct sound. Consider adding sound-absorbing materials like curtains, rugs, or acoustic panels to improve clarity.
Tip 6: Consider Auditory Health: Changes in hearing perception can indicate an underlying medical condition. If the issue persists despite addressing environmental and equipment factors, seek a hearing evaluation from a qualified audiologist. Gradual hearing loss or specific frequency deficits can alter the subjective experience of sound.
By systematically addressing potential sources of audio distortion, individuals can often restore clarity and enhance the overall listening experience. Implementing these measures can improve communication, enjoyment of audio entertainment, and overall awareness of environmental sounds.
The subsequent sections will delve into specific medical conditions that can contribute to alterations in auditory perception.
1. Earwax accumulation
Earwax, or cerumen, is a naturally occurring substance produced within the ear canal. While it serves a protective function, excessive accumulation can significantly impede sound transmission, resulting in a perceived lack of auditory clarity.
- Physical Obstruction of the Ear Canal
Cerumen buildup acts as a physical barrier, preventing sound waves from reaching the tympanic membrane (eardrum) effectively. The density and location of the earwax plug directly influence the degree of sound attenuation. Complete blockage leads to a substantial reduction in perceived volume and clarity.
- Frequency-Dependent Attenuation
The presence of earwax does not uniformly dampen all sound frequencies. Lower frequencies may be less affected than higher frequencies, leading to a distorted auditory experience where high-pitched sounds seem diminished or absent. This uneven attenuation contributes to a sensation of muffled hearing.
- Impact on Sound Localization
Earwax accumulation can affect the brain’s ability to accurately localize sound sources. Asymmetrical blockage between the two ears introduces discrepancies in sound arrival time and intensity, making it difficult to pinpoint the direction from which a sound originates.
- Interaction with Pre-existing Hearing Conditions
In individuals with pre-existing hearing loss, earwax accumulation can exacerbate the condition. The added obstruction compounds the existing auditory deficit, leading to a more pronounced perception of muffled sound and further impacting speech comprehension.
The impact of earwax on auditory perception underscores the importance of routine ear hygiene and professional cerumen management when necessary. The described attenuation, distortion, and localization issues all contribute to the subjective experience, thereby connecting “Earwax accumulation” directly to why sounds may seem indistinct or “why does everything sound muffled.”
2. Fluid in ear
The presence of fluid within the middle ear cavity significantly impedes the transmission of sound vibrations, consequently resulting in a perception of reduced auditory clarity. This phenomenon, often described as muffled hearing, arises due to the alteration of the impedance matching mechanism essential for efficient sound transfer from the air to the inner ear. In a healthy ear, the air-filled middle ear and the ossicles (malleus, incus, and stapes) act as an amplifier, compensating for the difference in impedance between the air and the fluid-filled inner ear. When fluid occupies the middle ear, this impedance matching is disrupted, requiring more energy for sound to travel, leading to sound dampening. For instance, individuals experiencing otitis media, a common middle ear infection, frequently report a sensation of muffled hearing due to the inflammatory fluid accumulation.
Furthermore, the type and viscosity of the fluid influence the extent of auditory impairment. Serous fluid, commonly associated with barotrauma or mild Eustachian tube dysfunction, may cause subtle sound alterations. Conversely, thick, purulent fluid characteristic of bacterial infections can significantly attenuate sound transmission across a wider frequency range. Clinically, audiometry reveals a conductive hearing loss, particularly affecting lower frequencies, in patients with middle ear effusion. The degree of hearing loss correlates with the amount and nature of the fluid present. The Eustachian tube, responsible for pressure equalization between the middle ear and the nasopharynx, plays a crucial role in preventing fluid accumulation. Dysfunction of this tube, often due to allergies or upper respiratory infections, predisposes individuals to middle ear effusions and subsequent auditory distortion.
In summary, fluid in the middle ear fundamentally alters the mechanics of sound transmission, causing the sound to seem faint and “why does everything sound muffled”. Recognizing the etiology of fluid accumulation, whether infectious, inflammatory, or related to Eustachian tube dysfunction, is paramount for effective intervention. Treatment strategies range from watchful waiting to antibiotic therapy or surgical intervention, all aimed at restoring normal middle ear function and auditory acuity. The implications extend beyond mere sound perception, affecting speech understanding, particularly in noisy environments, and potentially impacting cognitive development in children.
3. Hearing loss
Hearing loss, irrespective of its origin, often manifests as a perception of reduced auditory clarity. The experience is frequently described as if sounds are distant, attenuated, or lacking in distinctness, correlating directly with the sensation of a muffled auditory environment. This perceived muffling arises from the diminished ability to detect and process specific frequencies, hindering the accurate decoding of complex soundscapes. The severity and characteristics vary widely depending on the type, degree, and configuration of hearing loss.
Sensorineural hearing loss, resulting from damage to the inner ear or auditory nerve, typically leads to a generalized reduction in sound intensity across multiple frequencies, but disproportionately impacts higher frequencies crucial for speech clarity. Consequently, speech may be perceived as indistinct, lacking crispness, and difficult to understand, particularly in noisy environments. Conductive hearing loss, caused by obstructions or impairments in the outer or middle ear, similarly reduces the overall sound level reaching the inner ear. While amplification can sometimes mitigate the effects of conductive loss, the inherent distortion introduced by the impairment contributes to the sensation of a muffled auditory experience. For example, an individual with age-related hearing loss might report difficulty understanding conversation, describing voices as sounding unclear or as if they are speaking from behind a barrier. This scenario highlights the critical impact of hearing loss on the overall listening experience, emphasizing the connection to the subjective experience.
Early identification and management of hearing loss are essential for mitigating its impact on auditory perception and overall quality of life. The correlation between hearing loss and a degraded auditory environment underscores the importance of regular hearing evaluations and the utilization of appropriate amplification or other assistive technologies. Addressing hearing loss can significantly improve speech comprehension, reduce listening fatigue, and enhance overall environmental awareness. Left unaddressed, hearing loss causes “why does everything sound muffled”, affecting communication, potentially isolating individuals, and impacting their overall well-being.
4. Sensorineural damage
Sensorineural damage, affecting the inner ear (cochlea) or the auditory nerve, is a primary contributor to the perception of muffled or distorted sound. This type of damage disrupts the transduction of sound waves into electrical signals that the brain can interpret. The delicate hair cells within the cochlea, responsible for detecting different frequencies, can be damaged by factors such as noise exposure, aging (presbycusis), ototoxic medications, or genetic predispositions. When these hair cells are compromised, their ability to accurately transmit auditory information diminishes, leading to a distorted or incomplete representation of the sound reaching the brain. Consequently, individuals may perceive sounds as less clear, lacking in high-frequency components, or generally muffled. For example, a musician with noise-induced sensorineural hearing loss might find it increasingly difficult to discern subtle nuances in music, reporting that the overall sound lacks its former brilliance and clarity.
The specific pattern of sensorineural damage significantly influences the nature of the perceived auditory distortion. High-frequency hearing loss, a common consequence of noise exposure and aging, often results in difficulty understanding speech, particularly in noisy environments. The consonants, which carry essential information for speech intelligibility, are predominantly high-frequency sounds. Damage to the auditory nerve, although less common, can lead to a more profound and generalized form of auditory distortion, where sounds may seem both muffled and indistinct. Understanding the underlying mechanisms of sensorineural damage is crucial for developing effective strategies for prevention, early detection, and management. Audiological assessments, including pure-tone audiometry and speech discrimination testing, play a vital role in identifying the presence, type, and extent of sensorineural hearing loss.
In summary, sensorineural damage directly impairs the accurate processing of sound, leading to the subjective experience of “why does everything sound muffled.” The impact on auditory perception depends on the location and extent of the damage, ranging from mild high-frequency hearing loss to more severe and generalized auditory distortion. Early intervention, including hearing aids, cochlear implants, and auditory training, can help mitigate the effects of sensorineural damage and improve the overall quality of life for affected individuals. Prevention strategies, such as noise protection and careful medication management, are paramount in preserving auditory function and preventing the onset or progression of sensorineural hearing loss.
5. Acoustic neuroma
An acoustic neuroma, also known as a vestibular schwannoma, is a benign tumor that develops on the vestibulocochlear nerve, which connects the inner ear to the brain. This nerve is crucial for both hearing and balance, making any disruption to its function potentially impactful. As an acoustic neuroma grows, it can exert pressure on the nerve fibers responsible for transmitting auditory information, leading to a variety of auditory symptoms. One common manifestation of this pressure is a perceived reduction in auditory clarity. An individual might experience a sensation of muffled hearing, particularly in the affected ear, due to the tumor interfering with the nerve’s ability to accurately transmit sound signals to the brain. The distortion of these signals results in a degraded auditory experience, often described as if sounds are distant, indistinct, or lacking in their normal vibrancy. This type of hearing loss is typically sensorineural, meaning it arises from damage to the inner ear or the nerve itself. For instance, a patient diagnosed with an acoustic neuroma might initially report difficulty understanding conversations, especially in noisy environments, and describe sounds as being muffled or unclear. The insidious nature of the tumor’s growth often leads to a gradual onset of these auditory symptoms, making early detection challenging.
Beyond the direct pressure on the vestibulocochlear nerve, an acoustic neuroma can indirectly affect auditory perception by disrupting the function of nearby structures within the skull. As the tumor expands, it can compress the brainstem and other cranial nerves, potentially leading to further neurological deficits. These deficits can exacerbate the existing auditory problems, contributing to a more pronounced sensation of muffled hearing and overall auditory distortion. Furthermore, the surgical removal of an acoustic neuroma, while often necessary to prevent further neurological complications, can also impact auditory function. Depending on the size and location of the tumor, surgery may result in permanent hearing loss or tinnitus, both of which can contribute to a subjective experience. The likelihood of preserving hearing during surgery is influenced by factors such as the tumor size, the patient’s pre-operative hearing level, and the surgical approach used. Advanced surgical techniques, such as microsurgery and stereotactic radiosurgery, are aimed at minimizing damage to the vestibulocochlear nerve and preserving auditory function whenever possible.
In conclusion, an acoustic neuroma can lead to the sensation of muffled hearing through direct compression of the vestibulocochlear nerve, subsequent disruption of auditory signal transmission, and potential complications arising from tumor growth or surgical intervention. Early diagnosis, achieved through audiometry and imaging techniques such as MRI, is crucial for timely management and mitigation of auditory symptoms. The correlation between acoustic neuroma and degraded auditory perception underscores the importance of considering neurological causes in the differential diagnosis of hearing loss. Understanding the mechanisms by which an acoustic neuroma impacts auditory function enables healthcare professionals to provide appropriate treatment and support to affected individuals. The challenge lies in balancing tumor control with the preservation of hearing and neurological function, requiring a multidisciplinary approach involving neurosurgeons, audiologists, and other specialists.
6. Equipment malfunction
Auditory equipment, including headphones, speakers, and amplifiers, relies on the precise conversion and transmission of electrical signals into audible sound waves. When these devices malfunction, their ability to accurately reproduce sound diminishes, often resulting in the perception that sounds are indistinct or “muffled.” A faulty speaker driver, for instance, may exhibit a restricted frequency response, failing to reproduce high-frequency components vital for clarity. This selective attenuation of specific frequencies creates a sensation of altered sound quality, where the overall audio lacks detail and crispness. Similarly, damaged wiring or loose connections within headphones can introduce signal degradation, leading to intermittent or consistently distorted audio output. The result is a subjective experience of reduced fidelity, characterized by the inability to clearly discern individual instruments or vocal nuances within a musical piece. The impact is not limited to consumer-grade audio equipment; professional recording and broadcast systems are equally susceptible to malfunctions that compromise sound quality, affecting the final auditory product.
The role of equipment malfunction in generating a “muffled” sound is further exacerbated by the ubiquity of digital signal processing (DSP) in modern audio devices. While DSP can enhance audio quality, faulty algorithms or improperly configured settings can introduce unintended artifacts, such as excessive compression or filtering. These artifacts can smear transient details, reduce dynamic range, and contribute to a sense of auditory compression, all of which manifest as a loss of clarity. Regular maintenance, proper calibration, and the use of high-quality components are essential for preventing equipment malfunctions and maintaining optimal audio performance. The ability to diagnose and address such issues requires an understanding of audio engineering principles and the operational characteristics of the specific devices involved. Furthermore, the increasing complexity of audio systems necessitates the use of specialized diagnostic tools to identify and isolate the sources of audio distortion.
In summary, equipment malfunction represents a significant factor in the perception of reduced auditory clarity. The inability of faulty devices to accurately reproduce sound waves results in a subjective experience of muffled audio. Addressing this issue requires a systematic approach to troubleshooting, including the inspection of components, the verification of signal paths, and the calibration of settings. Understanding the potential for equipment-related auditory distortions is critical for maintaining audio fidelity across a wide range of applications, from personal listening to professional audio production, addressing the key phrase “why does everything sound muffled.”
7. Auditory processing disorder
Auditory processing disorder (APD) disrupts the brain’s ability to effectively interpret auditory information, even when hearing sensitivity is normal. The sounds themselves may be detected, but the brain struggles to organize, analyze, and understand them. This neurological inefficiency can manifest as a perceived lack of auditory clarity. Individuals with APD may report that speech sounds slurred or indistinct, resembling a “muffled” auditory experience. The distortion is not due to a physical blockage or impairment in the ear but rather to a breakdown in the central auditory nervous system’s processing capabilities. For instance, a child with APD might struggle to differentiate between similar-sounding words like “bat” and “pat,” leading to misinterpretations and communication difficulties. This exemplifies that APD can be a significant contributing factor.
The components of auditory processing affected in APD can include auditory discrimination (differentiating between sounds), auditory figure-ground discrimination (distinguishing sounds from background noise), auditory memory (remembering auditory information), and auditory sequencing (understanding the order of sounds). Deficits in any of these areas contribute to a distorted perception of auditory input. In a classroom setting, a student with poor auditory figure-ground discrimination may have difficulty focusing on the teacher’s voice due to the distracting background noise. The teacher’s voice may seem distant or muffled, even if the student is sitting close by. Practical applications of this understanding include the implementation of strategies such as preferential seating, the use of assistive listening devices, and targeted auditory training exercises aimed at improving specific auditory processing skills.
In summary, APD causes “why does everything sound muffled” through neurological inefficiency, directly impacting how the brain interprets sound. The experience differs from hearing loss as the sound itself is detected, but the processing is flawed. Early identification and intervention are crucial to mitigate the effects of APD on academic performance, communication skills, and overall quality of life. A key challenge lies in differentiating APD from other conditions with overlapping symptoms, such as attention-deficit/hyperactivity disorder (ADHD) and language impairments, requiring comprehensive audiological and neuropsychological assessments to establish an accurate diagnosis. The connection to the broader theme lies in recognizing that a perceived “muffled” auditory environment is not always indicative of a peripheral hearing problem but can stem from central auditory processing deficits.
Addressing Auditory Perception Issues
The following section addresses common inquiries regarding diminished auditory clarity, a condition often described as if everything sounds muffled. These questions and answers aim to provide clear and informative insights into potential causes and remedies.
Question 1: What are the primary reasons for a sudden onset of reduced auditory clarity?
Sudden reductions in auditory clarity often result from temporary conditions affecting the ear. Common causes include cerumen impaction, middle ear infections, exposure to sudden loud noises, or barotrauma due to rapid changes in air pressure. In rare cases, sudden sensorineural hearing loss may be the cause and requires immediate medical attention.
Question 2: How does cerumen accumulation contribute to diminished sound quality?
Cerumen, or earwax, can physically obstruct the ear canal, impeding sound waves from reaching the eardrum. The density and location of the cerumen plug determine the degree of sound attenuation, often selectively impacting higher frequencies essential for speech clarity. Removal of the cerumen typically restores normal auditory acuity.
Question 3: What role does the Eustachian tube play in maintaining auditory clarity?
The Eustachian tube connects the middle ear to the nasopharynx, equalizing pressure between the middle ear and the external environment. Dysfunction of the Eustachian tube, often caused by allergies or upper respiratory infections, can lead to negative pressure in the middle ear and fluid accumulation, both of which impair sound transmission and reduce auditory clarity.
Question 4: Can certain medications impact auditory perception?
Yes, some medications are ototoxic, meaning they can damage the inner ear and auditory nerve. These medications can cause tinnitus, hearing loss, or a distorted perception of sound, including the sensation that everything sounds muffled. Individuals taking potentially ototoxic medications should undergo regular hearing monitoring.
Question 5: How can environmental factors affect the perceived clarity of sound?
Environmental factors such as excessive noise, reverberation, and poor acoustics can significantly impair auditory perception. High levels of background noise mask quieter sounds, making it difficult to discern details. Reverberation and echoes distort sound waves, reducing clarity and intelligibility.
Question 6: When should a medical professional be consulted regarding reduced auditory clarity?
A medical professional should be consulted if reduced auditory clarity persists for more than a few days, is accompanied by pain or drainage from the ear, occurs suddenly and without apparent cause, or is associated with other neurological symptoms. Prompt evaluation can identify underlying medical conditions requiring treatment and prevent further auditory damage.
Maintaining awareness of potential causes and seeking timely intervention are crucial for preserving optimal auditory function. Persistent or unexplained changes in auditory perception warrant professional evaluation.
The subsequent section will explore the role of technology in both contributing to and mitigating auditory perception issues.
Concluding Remarks on Reduced Auditory Clarity
The preceding exploration has elucidated diverse factors contributing to the subjective experience of “why does everything sound muffled.” Physical obstructions, middle ear pathology, sensorineural damage, neurological conditions, equipment malfunctions, and auditory processing disorders each represent distinct mechanisms by which auditory fidelity can be compromised. Identifying the specific etiology is paramount for implementing effective interventions.
The multifaceted nature of auditory perception underscores the importance of a comprehensive approach to diagnosis and management. Persistent or unexplained alterations in auditory clarity warrant thorough investigation by qualified healthcare professionals. Proactive measures, including preventative strategies and timely intervention, can mitigate the impact of impaired auditory perception on communication, quality of life, and overall well-being.


![Why Does Your Beats Pro Sound Muffled? [FIX] Best Mufflers for Cars & Trucks | Performance, Sound & Durability Upgrades Why Does Your Beats Pro Sound Muffled? [FIX] | Best Mufflers for Cars & Trucks | Performance, Sound & Durability Upgrades](https://dnamufflers.com/wp-content/uploads/2026/02/th-524-300x200.jpg)