A vehicle component designed to reduce the noise produced by the engine’s combustion process. This element is typically installed as part of a complete system that channels exhaust gases away from the engine. One particular brand specializing in this component is known for its performance and sound characteristics.
The implementation of such a system offers a refined auditory experience, diminishing disruptive engine clamor and adhering to regulatory noise limitations. Furthermore, these systems can enhance engine efficiency by optimizing exhaust gas flow, which, in turn, can contribute to improved vehicle performance. Throughout automotive history, advancements in design and materials have led to more effective and durable examples.
Understanding the role and advantages of this critical component is crucial for enthusiasts seeking to optimize their vehicle’s auditory signature and performance characteristics. Further discussion will delve into specific attributes, installation considerations, and the overall impact on driving dynamics.
Essential Considerations
The subsequent points offer practical guidance for individuals considering the installation or maintenance of a vehicle’s exhaust silencing system.
Tip 1: Material Selection: Consider the composition of the system. Stainless steel provides superior corrosion resistance and longevity compared to aluminized steel, although it carries a higher initial cost.
Tip 2: Professional Installation: While some installations are straightforward, engaging a qualified technician ensures proper fitment, avoiding potential exhaust leaks or structural damage.
Tip 3: Sound Level Compliance: Verify adherence to local noise regulations. Systems exceeding permissible decibel levels can result in fines and vehicle impoundment.
Tip 4: Routine Inspection: Regularly examine the system for signs of corrosion, damage, or loose connections. Address any issues promptly to prevent escalation and potential safety hazards.
Tip 5: Performance Mapping: On modified engines, consider dyno-tuning the ECU to best match the new exhaust characteristics.
Tip 6: System Compatibility: Ensure that the chosen system is specifically designed for the target vehicle’s make, model, and year. Incompatible components can lead to performance degradation or mechanical complications.
Adherence to these guidelines promotes optimal performance, longevity, and compliance with applicable regulations.
The following section will offer insights into related considerations and address potential performance implications.
1. Sound Attenuation
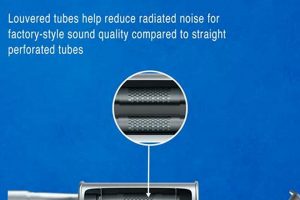
The primary function of an exhaust system component is sound attenuation, mitigating the intense noise generated by internal combustion engines. The “brand name” part achieves this through a combination of internal baffling, resonance chambers, and sound-absorbing materials. These elements disrupt and redirect sound waves, converting acoustic energy into thermal energy. Without effective sound attenuation, vehicles would produce excessive noise pollution, violating regulations and negatively impacting the environment.
The engineering of sound attenuation within the system directly influences the vehicle’s acoustic signature. Different designs produce distinct sound profiles, ranging from subtle reduction to a more aggressive tone, while still adhering to legal noise limits. The design choices include specific chamber volumes, baffle configurations, and insulation properties. These design choices impact the overall noise reduction and tonal quality. A vehicle with an improperly designed, or damaged sound attenuation system will experience increased noise levels, potentially attracting legal penalties.
In summary, sound attenuation represents a core design principle and functional attribute. Efficient reduction not only assures compliance but also impacts vehicle usability and driver/public perception. Understanding the connection between sound attenuation and the component allows for selection of the appropriate system.
2. Material Durability
The longevity and sustained functionality of an exhaust system component directly hinge on the materials employed in its construction. Material durability, therefore, is not merely a feature but a fundamental necessity, influencing the component’s lifespan, performance consistency, and overall value.
- Corrosion Resistance
Exhaust systems are subjected to extreme temperature fluctuations, moisture, road salts, and acidic condensates generated during combustion. The capacity of the component’s constituent materials to resist corrosion dictates its ability to withstand these hostile conditions, preventing premature failure and maintaining structural integrity. Stainless steel alloys, such as 304 or 409, offer superior corrosion resistance compared to aluminized steel, but are costlier. This difference in corrosion resistance is a critical factor in determining the long-term viability of the component in diverse operating environments.
- Thermal Stability
The cyclical heating and cooling of an exhaust system induce thermal stress within its materials. The ability of these materials to maintain their mechanical properties at elevated temperatures is crucial for preventing deformation, cracking, and eventual failure. Materials with high thermal stability, such as titanium or certain grades of stainless steel, are less susceptible to these stresses, resulting in a more durable and reliable component.
- Weld Integrity
Welding is a critical process in the fabrication of exhaust systems, and the integrity of these welds directly impacts the overall durability of the component. Welds must exhibit sufficient strength, ductility, and corrosion resistance to withstand the stresses imposed by thermal cycling, vibration, and exposure to corrosive elements. Poorly executed or incompatible welding techniques can introduce stress concentrations and corrosion points, significantly reducing the component’s lifespan.
- Impact Resistance
While not the primary design consideration, the ability of an exhaust system to withstand impacts from road debris or minor collisions can contribute to its overall durability. Thicker gauge materials and robust construction techniques can mitigate the risk of damage from such events, extending the component’s service life. Understanding impact resistance ensures continued reliability in real-world driving conditions.
The selection of durable materials is a fundamental aspect of exhaust component design, impacting not only the system’s lifespan but also its performance characteristics and overall value proposition. The initial cost of using premium materials may be higher, but this investment often translates into long-term savings through reduced maintenance, repair, and replacement costs.
3. Performance Optimization
Performance optimization, when considered in the context of exhaust systems, entails engineering a system to maximize engine efficiency, power output, and responsiveness. The selection and integration of components, directly influences the flow dynamics of exhaust gases, which subsequently impacts engine performance. This section delves into the multifaceted connection between exhaust system design and engine performance characteristics.
- Exhaust Gas Velocity and Scavenging
Exhaust systems are designed to optimize exhaust gas velocity, facilitating efficient scavenging of combustion byproducts from the engine cylinders. Tuned exhaust systems, including specific types, can generate a scavenging effect, creating a negative pressure wave that aids in drawing out exhaust gases and improving cylinder filling during the intake stroke. An enhanced scavenging effect increases the volumetric efficiency of the engine, resulting in improved power and torque output.
- Backpressure Reduction
Excessive backpressure in an exhaust system hinders the expulsion of exhaust gases, reducing engine efficiency. The system’s design aims to minimize backpressure while maintaining adequate flow velocity. Larger diameter piping and optimized muffler designs contribute to reducing backpressure, enabling the engine to breathe more freely and produce more power. A reduction in backpressure can also lead to improved fuel economy, as the engine requires less energy to expel exhaust gases.
- Resonance Tuning and Wave Propagation
Advanced exhaust systems utilize resonance tuning principles to manipulate pressure wave propagation within the system. By carefully designing the length and diameter of exhaust pipes, engineers can create constructive interference of pressure waves at specific engine speeds, enhancing cylinder filling and improving torque output. Resonance tuning is particularly effective in optimizing performance within a defined RPM range, tailoring the engine’s power delivery characteristics to specific driving needs.
- Catalytic Converter Efficiency and Flow
Catalytic converters, while primarily intended to reduce emissions, can also impact exhaust flow and engine performance. High-flow catalytic converters are designed to minimize backpressure while maintaining effective emissions control. These converters utilize larger cell densities and optimized flow paths to reduce flow restriction, enabling the engine to breathe more freely and maintain optimal performance levels. The implementation of high-flow catalytic converters is a crucial element in achieving performance optimization without compromising environmental compliance.
The integration of these design considerations in the fabrication of an exhaust system directly impacts engine performance. These systems are designed to optimize exhaust gas flow, reduce backpressure, and leverage resonance tuning to enhance power, torque, and fuel efficiency. Understanding the intricate relationship between exhaust system design and engine dynamics is essential for individuals seeking to maximize their vehicle’s performance potential while adhering to emissions regulations.
4. Brand Reputation
A brand’s reputation significantly influences consumer perception and purchasing decisions, particularly in specialized automotive components such as exhaust systems. The established credibility of a manufacturer directly correlates with perceived product quality, reliability, and performance. When considering “Remus exhaust muffler,” the brand’s history of innovation, materials quality, and performance results critically shapes consumer trust. A positive brand image provides assurance of value and mitigates perceived risk in the purchasing decision. For example, a brand with a demonstrated history of durability and consistent performance fosters confidence, resulting in higher demand and premium pricing.
Examining customer testimonials, independent product reviews, and professional assessments reveals the practical impact of brand standing. A brand recognized for engineering precision and meticulous quality control typically garners positive feedback regarding product fitment, sound characteristics, and performance gains. Conversely, a brand lacking a strong reputation may face skepticism, even if the technical specifications of its products appear similar to established competitors. The market often reflects this disparity through varied pricing and consumer adoption rates. The effect goes beyond initial sales, influencing long-term customer loyalty and repeat purchases.
Ultimately, the established reputation of a manufacturer like Remus directly informs consumer expectations and purchasing behaviors. A reputable brand serves as a proxy for quality and performance, reducing perceived risk and influencing buying decisions. While technical specifications and features are important, the intangible value of a strong brand often serves as a decisive factor for informed consumers.
5. Vehicle Compatibility
The successful integration of aftermarket components, such as exhaust systems from manufacturers, hinges critically on vehicle compatibility. Proper fitment, performance alignment, and regulatory compliance are all predicated on selecting a system specifically engineered for the target vehicle. Incompatibility can lead to performance degradation, mechanical complications, and even safety hazards.
- Model-Specific Design
Exhaust systems are often designed to accommodate the unique chassis configuration, engine specifications, and mounting points of specific vehicle models. A system intended for a sedan may not fit properly on a coupe or SUV due to differences in wheelbase, ground clearance, or exhaust routing. Incorrect fitment can result in exhaust leaks, structural stress, and reduced ground clearance, compromising both performance and safety. For example, installing an exhaust system designed for a rear-wheel-drive vehicle on an all-wheel-drive model can interfere with the driveline components, leading to mechanical damage.
- Engine Compatibility
Engine displacement, cylinder configuration, and exhaust port design significantly influence the flow dynamics and performance characteristics of an exhaust system. A system designed for a four-cylinder engine may be inadequate for a V6 or V8, resulting in excessive backpressure and reduced power output. Conversely, an exhaust system with oversized piping can reduce exhaust gas velocity, negatively impacting low-end torque. Engine compatibility is a critical factor in achieving optimal performance and preventing engine damage. Performance mapping on a dynometer is always recommended.
- Emissions Compliance
Exhaust systems must comply with local and federal emissions regulations, including those pertaining to catalytic converters and noise levels. An incompatible system may lack the necessary catalytic converters or mufflers to meet these requirements, leading to fines and vehicle inspection failures. Modifying or removing emissions control devices is often illegal and can negatively impact air quality. Ensuring emissions compliance is both a legal obligation and an ethical responsibility.
- Electronic Control Unit (ECU) Integration
Modern vehicles rely on sophisticated ECUs to manage engine parameters and optimize performance. The installation of an aftermarket exhaust system can alter exhaust gas flow and sensor readings, potentially disrupting the ECU’s ability to properly control fuel delivery, ignition timing, and other critical functions. Recalibrating the ECU, or installing a supplementary control module, may be necessary to ensure optimal performance and prevent engine damage following the installation of a new exhaust system. It is recommended to seek a professional to assist in these matters.
Understanding the intricacies of vehicle compatibility is paramount when selecting an aftermarket exhaust system, such as those available from Remus. Prioritizing proper fitment, engine compatibility, emissions compliance, and ECU integration ensures optimal performance, reliability, and adherence to legal requirements. Failure to adequately address these considerations can lead to costly repairs, performance degradation, and regulatory violations.
6. Aesthetic Design
Aesthetic design, in the context of components like a “Remus exhaust muffler,” extends beyond mere surface appearance; it represents a deliberate integration of form and function, influencing consumer perception and brand identity. The visual characteristics of an exhaust component contribute to the vehicle’s overall styling, signaling performance capabilities and reflecting the owner’s preferences. The design elements include material finishes (polished stainless steel, carbon fiber accents), shape and profile, weld quality, and the prominence of branding elements. These characteristics directly impact the perceived value and desirability of the product.
The aesthetic considerations in the design of a Remus exhaust component frequently mirror the performance-oriented image of the vehicle it is intended for. Systems designed for sports cars and high-performance vehicles often feature aggressive styling cues, such as quad exhaust tips or prominent diffusers, communicating the component’s performance-enhancing capabilities. In contrast, systems designed for luxury vehicles may emphasize a more refined and understated aesthetic, blending seamlessly with the vehicle’s existing styling while subtly enhancing its visual appeal. Brand identity is also a significant factor; the careful placement of logos and brand-specific design elements reinforces brand recognition and conveys a sense of quality and prestige. For instance, the precise angles and curvature of the exhaust tips, or the use of laser-etched logos, can differentiate a brand’s product from competitors, solidifying its position in the market.
The aesthetic design of an exhaust component carries practical significance because it directly affects consumer perception and brand loyalty. A well-designed component enhances the vehicle’s visual appeal, contributing to the owner’s satisfaction and pride of ownership. Moreover, a consistent and recognizable aesthetic across a product line reinforces brand identity and builds trust with consumers. The fusion of form and function represents a strategic imperative for manufacturers seeking to distinguish their products in a competitive market, demonstrating a commitment to both performance and visual excellence.
Frequently Asked Questions
The following addresses common inquiries and misconceptions regarding a vehicle’s exhaust system and performance characteristics.
Question 1: Does installing an aftermarket exhaust system void the vehicle’s warranty?
The installation of an aftermarket exhaust system does not automatically void a vehicle’s warranty. However, if the aftermarket component directly causes a failure of a covered component, the warranty claim may be denied. Consumers should consult with their vehicle manufacturer or dealer to fully understand warranty implications. It is essential to ensure that modifications adhere to applicable regulations and do not demonstrably compromise the vehicle’s integrity.
Question 2: What is the expected lifespan of a stainless steel exhaust system?
The lifespan of a stainless steel exhaust system depends on several factors, including the grade of stainless steel used, driving conditions, and maintenance practices. Under typical operating conditions, a properly installed and maintained stainless steel system can last for 10 years or more. Exposure to corrosive elements, such as road salt, can shorten its lifespan. Regular inspection and cleaning can prolong the system’s durability.
Question 3: How does an aftermarket exhaust system affect vehicle emissions?
The effect of an aftermarket exhaust system on vehicle emissions varies depending on its design and the presence of functioning catalytic converters. A properly designed system with compliant catalytic converters should not significantly increase emissions. However, removing or modifying catalytic converters is illegal in many jurisdictions and can result in increased emissions and regulatory penalties. A vehicle should be professionally tested to ensure that it meets emissions standards after any modifications.
Question 4: Can an aftermarket exhaust system improve fuel economy?
An aftermarket exhaust system may contribute to improved fuel economy if it reduces backpressure and enhances engine efficiency. By facilitating smoother exhaust gas flow, the engine may require less energy to expel exhaust gases, potentially leading to a slight improvement in fuel economy. However, any gains in fuel economy are typically modest and may not be noticeable under all driving conditions. Driving style and vehicle maintenance practices also play a significant role in fuel consumption.
Question 5: Are all aftermarket exhaust systems street legal?
Not all aftermarket exhaust systems are street legal. Many jurisdictions have regulations governing noise levels and emissions standards. Systems that exceed permissible noise limits or lack required emissions control devices may be illegal to operate on public roads. Consumers are responsible for ensuring that any aftermarket exhaust system they install complies with all applicable local, state, and federal regulations. The system should be labeled as compliant.
Question 6: What are the potential drawbacks of installing an aftermarket exhaust system?
Potential drawbacks of installing an aftermarket exhaust system include increased noise levels, potential emissions non-compliance, and the risk of reduced low-end torque if the system is not properly designed. A poorly designed system can also create drone, which is an unpleasant resonance at certain engine speeds. It is crucial to select a reputable brand and ensure proper installation to minimize these potential drawbacks.
It is important to consider these aspects when assessing benefits and potential compliance, to make the correct choices for the specific requirements and expectations.
The following section will offer insights into related considerations and address potential performance implications.
In Summary
The preceding examination of a component designed for vehicle exhaust systems, specifically those manufactured by Remus, has underscored several critical considerations. These range from the fundamental principles of sound attenuation and material durability to the more nuanced aspects of performance optimization, brand reputation, and vehicle compatibility. A comprehensive understanding of these factors is paramount for making informed decisions regarding exhaust system upgrades or replacements. Each element contributes to the overall efficacy and long-term value of the selected system.
The careful consideration of these factors ensures proper functionality, longevity, regulatory compliance, and optimal performance of the vehicle. Whether seeking to enhance the vehicle’s auditory signature or improve its overall performance, a thorough evaluation of available options, grounded in technical understanding and practical knowledge, will yield the most satisfactory results. Continued advancements in materials science and engineering will undoubtedly lead to further refinements in exhaust system design, offering even greater opportunities for vehicle customization and performance enhancement in the years to come.